Modular Content For Pharma
Mark Violi | 06.03.25
Originally published in MedAdNews, June 2025
Introduction
As the pharmaceutical industry responds to growing customer demand for information and pressures to contain costs and improve return on investments, it’s no surprise many have embraced Modular Content as a strategy to create, manage, and distribute personally relevant content at scale efficiently.
“Modular content” refers to the creation of standalone, reusable “content modules” that can be mixed, matched, and customized based on specific requirements. These modules can be tailored for different customer segments, market needs, target audiences, and communication channels. The approach promises advantages in terms of efficiency, personalization, scalability, reduced costs and time.
However, rolling out a successful modular content strategy in a complex, regulated industry requires more than just the creation of content. It demands a holistic approach involving planning, training, regulatory buy-in, process implementation, change management, and technology.
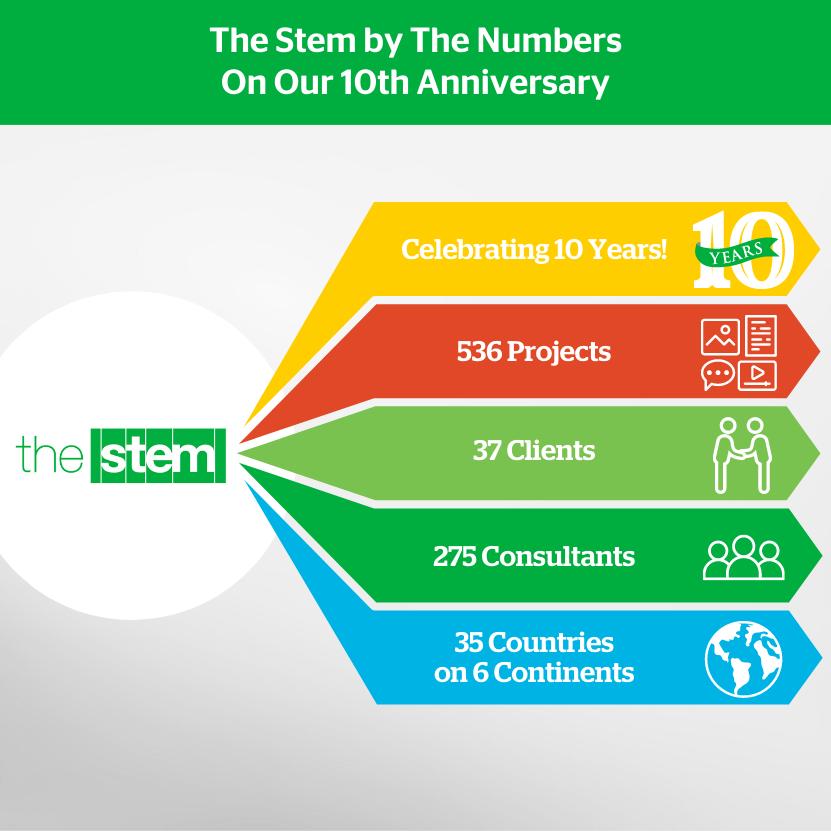
Early adopters of modular content have been building capabilities for several years, but many organizations are just beginning. This article shares key lessons learned from leaders in the field so new adopters can learn from the pitfalls they encountered and benefit from their successes. To provide a well-rounded perspective, we consulted members of The Stem network and key industry leaders including Merck (Brian Everhart), Grunenthal (Mubasher Hassan) and Joe Falcone (The Stem, formerly Bristol Myers Squibb). Their insights highlight critical lessons learned and strategies in transitioning to a modular content way of working.
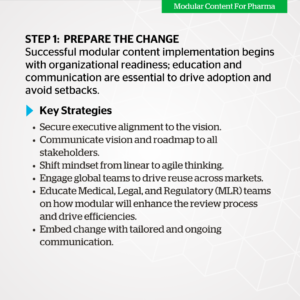
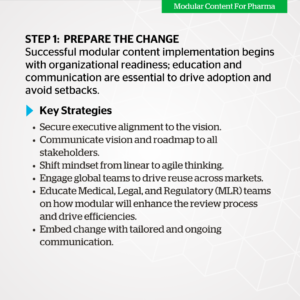
Step 1: Prepare the Change
One of the most common pitfalls in implementing modular content is underestimating the preparation and change required. Without properly planning, organizations risk inefficiencies, compliance setbacks, and duplication of effort.
Resistance to change is common. Whether its internal teams struggling with new workflows or regulatory teams adopting a new way of reviewing content, a structured approach to change is necessary.
A: Executive Alignment
Leadership must be fully aligned with the long-term benefits of modular content, since it is resource-intensive and time-consuming in the beginning. It’s critical for senior leaders to actively support the initiative and drive it forward. This support should extend to MLR (Medical, Legal, Regulatory), IT, and Brand/Marketing.
Joe Falcone explains why leadership buy-in is critical: “Leadership saw modular content as essential, but the story wasn’t initially clear. Without a well-communicated vision, people just brushed it aside….It moved at a slow crawl for two years because leadership wasn’t fully ready and the right resources took more time to put in place than they had hoped. They wanted other organizational changes to settle first… Without a strong, well-communicated vision and structure, people just saw it as another initiative to set aside.”

Change communication should begin with leadership. Key stakeholders in marketing, medical, legal, regulatory, and IT must understand the broader vision, the benefits, and the challenges involved. “Leaders need to know what’s changing, why it matters, and how to support their teams,” Falcone emphasized.
A well-defined vision must be reinforced through clear messaging, ongoing engagement, and structured education tailored to each function’s role.
B: Ensure Mindset Shift Is Understood Among Key Stakeholders
\Shifting to modular content requires a fundamental change in how stakeholders—across global and local teams—approach content planning, creation, and approval.
Hassan explains: “Traditionally, content is created in a linear way, but with modular content, each module must represent a single, standalone key message. Adapting to this way of thinking doesn’t happen overnight.
Each function needs to rethink traditional workflows and embrace a more strategic, reusable content approach.
- Global Teams: Must shift from static content created in silos to dynamic content modules that are re-used across markets.
- Brand Teams: Need to embrace speed and efficiency gains of modular content, particularly in how they brief agencies. Rather than commissioning full creative pieces, teams request modular components that can be assembled and adapted quickly for different channels, segments, and markets.
- Medical, Legal, and Regulatory (MLR) Teams: Need to embrace a new way of working: when fully assembled content is reviewed and approved, they will also be setting business rules and approving the Modules used to reuse these assets in the future. This will enable them to recognize previously reviewed modulars when incorporated into the next asset submission. It also gives them greater control and traceability across campaigns while streamlining the review process.
By proactively addressing these mindset shifts early, teams can align on the new ways of working, accelerating adoption and minimizing friction during implementation.
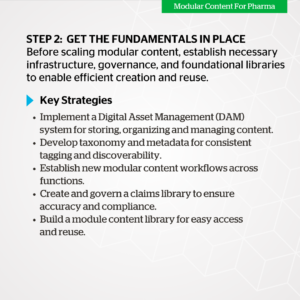
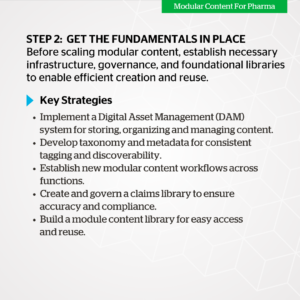
Step 2: Get the Fundamentals in Place First
A. Set Up Foundational Capabilities
To successfully implement modular content in pharma, organizations must first establish the core infrastructure that enables scalability, efficiency, and compliance. This foundational phase ensures that content is properly structured, workflows are optimized, and technology is in place to support seamless content reuse.
B. Build Tagging/MetaData/Taxonomy – Lexicon
Develop a structured system to categorize and organize content efficiently. Define a standardized taxonomy and metadata framework that aligns with business objectives and user needs. Ensure consistency in tagging across content types to facilitate discoverability, reuse, and personalization.
C. Select a Content Authoring Partner
Identify and collaborate with a content authoring platform or partner that aligns with your modular content strategy. Consider capabilities such as structured content creation, AI-powered automation, and seamless integration with existing systems. Ensure the partner supports multi-channel content delivery and version control.
D. Establish new workflows
Design and implement streamlined workflows to support modular content creation, management, and distribution. Define processes for:
- Ingesting and organizing new content within the library
- Breaking down content into reusable modules
- Harvesting and repurposing existing assets
- Reviewing and approving content
E. Enable a Claims Library
Set up a centralized claims library to ensure accuracy, compliance, and consistency in content messaging. Establish governance rules, verification processes, and integration with content management systems. Ensure seamless retrieval and tagging of approved claims for easy reuse across various content modules.
Hassan underscores the critical role of establishing a claims library as a foundation for modular content implementation: “Digital claims are a key aspect of modular content. At the time, we didn’t have them enabled, so the project became three initiatives in one: implementing digital claims, modular content, and a new co-creation model. For smaller organizations, I’d strongly recommend starting with digital claims first—don’t jump into modular content without that foundation.”
Enable a Module/Content Library
Establish a structured module library. A Module/Content Library is a centralized, organized repository of previously reviewed content modules (and the individual elements within those modules – referenced claims, images, and reusable text blocks) that can be easily accessed, localized, and reused by markets or teams across different regions. It serves as the backbone of the modular content process, enabling efficient creation and adaptation of final assets. By using reusable modules, teams can quickly assemble tailored, compliant, and brand-consistent content without having to start from scratch for each new market or campaign, ensuring faster time-to-market and consistency across global communications.
A key challenge with building this library upfront is overcoming the perception of “double work,” as markets must continue publishing content while also building modular assets. A more effective approach is to have agencies extract modules from existing content, allowing the library to grow organically without disrupting workflows.
Hassan (Grünenthal) shared insights on their approach to building a library of modules:
“To really see these benefits, you need a library of modules. Once you have that, you can start leveraging them effectively. However, building that initial library is a huge undertaking. Markets might feel like they are putting in a lot of effort without immediate results because while they are creating modules, they are also publishing content. It can feel like double the work. Initially, we thought markets should create their own library, but we quickly revised that approach.
Instead, we asked markets to continue creating content as usual while the agencies they worked with were responsible for developing modules from that content. This way, as content was produced, the module library grew naturally – and this approach proved highly effective.”
Establish DAM, if not already in place
A Digital Asset Management (DAM) system – a centralized platform for storing, organizing, and managing digital content – is essential for the successful implementation of modular content in pharma. If not already in place, it should be prioritized to ensure efficient storage, retrieval, and governance of modular assets.
Key considerations when establishing or optimizing a DAM system include:
- Structured Metadata & Tagging: Ensure all modular assets are properly tagged for easy searchability and reuse across regions and teams.
- Version Control & Compliance: Track asset updates and approvals to maintain compliance with regulatory requirements.
- Integration with Other Systems: Connect the DAM with content management systems (CMS), Medical, Legal, and Regulatory (MLR) platforms, and workflow automation tools for seamless content lifecycle management.
- Governance & Access Control: Define permissions to ensure appropriate access for different teams while maintaining content integrity and compliance.
A well-implemented DAM enables content efficiency, global consistency, and regulatory compliance, making it a cornerstone of any modular content strategy in pharma.
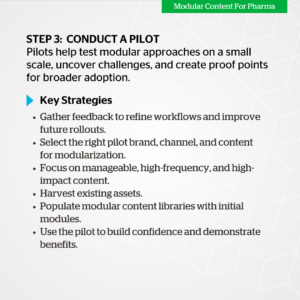
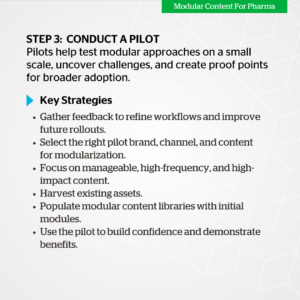
Step 3: Conduct a Pilot
Begin the implementation of your modular content strategy with a small scope pilot. Testing the process with a pioneer market and a limited number of brands allows teams to try modular approaches in a controlled environment, build confidence, uncover roadblocks, and create early success stories to fuel broader adoption.
A. Select the Right Pilot Brand, Channel, and Content
Choosing the right pilot can make or break the initiative. It’s essential to begin with a brand that is open to experimentation, has a manageable volume of content needs, and ideally, has leadership support.
When selecting a channel for your pilot, prioritize one that offers high content velocity, clear metrics, and manageable complexity – such as email or banner. These channels often require frequent updates and localization, making them ideal for testing modular content’s ability to improve speed, consistency, and reuse.
Choose content that is high-impact, frequently reused, and lends itself well to modularization – such as core brand messages, product value propositions, or disease education materials. Ideal pilot content should be relatively stable (to avoid frequent changes during the pilot) but broad enough to apply across channels or markets.
B. Harvest Existing Content
Start by mining existing brand assets for reusable content elements. Review slide decks, emails, sales materials, and web copy to identify frequently used messages, claims, and visuals.
This step is not only efficient, but also helps ease stakeholders into the modular approach by showing how existing content can be repurposed rather than reinvented.
C. Seed Claims and Modular Library
With content harvested, the next step is to populate a claims library and a modular content library. Begin with a minimal viable library (MVL) that includes:
- Pre-approved claims, correctly referenced and tagged with relevant metadata
- Core messaging modules categorized by channel and content type

Step 4: Engage the Brands & Markets with Rollout
With the foundations established and a pilot plan in place, it’s time to bring modular content to life across brands and markets. This step focuses on activating teams, scaling the approach, and embedding modular ways of working into day-to-day content operations. Success hinges on close collaboration between global and local teams, co-creation of content, and agile training to build confidence and drive adoption.
A: Co-Create with Brands and Markets
Global Therapeutic Areas (TAs) play a central role in modular content strategies, as they are responsible for creating content that meets both brand objectives and local market needs. To ensure effective adoption, global and local brand teams must collaborate from the outset. Close alignment and continuous communication between these teams ensure that content is both relevant and delivered on time, making it easier for local teams to adapt it to their specific markets.
Hassan reinforced this point: “We started co-creating content with markets instead of forcing a global-first approach. This made adoption much smoother. Now, regarding how global and local modules work together: we have both established brands and growth brands. For established brands, most content is already created, and global provides a basic toolkit for markets. Some markets, being more advanced, have additional needs, so they create their own local modules. The delta between global content and market-specific needs is covered by local module creation.”
Shifting away from a top-down content distribution model, Grünenthal embraced a more collaborative approach: “We moved away from the ‘global dumps content onto markets’ model. Instead, we adopted co-creation—where global works with markets to develop modules that are immediately relevant. This makes content more localized and effective.”

B: Be Agile in Training
One of the most common oversights in modular content adoption is underestimating the need for continuous, and right-sized training. As teams transition to modular content, many struggle to understand how modular components fit together, making structured and ongoing education essential.
Effective training should start with the fundamentals, focusing on the core principles of modular content—its flexibility, reusability, and potential for personalization. Rather than overwhelming teams with complex guidelines upfront, organizations should take a phased approach, gradually introducing more advanced topics as processes mature. Training materials must remain adaptable and continuously updated to reflect evolving modular content strategies and platform enhancements. Given the dynamic nature of modular content, resources should be designed to accommodate ongoing changes and improvements seamlessly – in essence, Modular training should be created.
To sustain adoption and engagement, training should be delivered in bite-sized, ongoing sessions rather than one-time, intensive programs. Regular reinforcement and providing teams on-demand resources for just-in-time needs helps teams stay aligned and maintain momentum as they become more comfortable with modular workflows.
Brian Everhart (Merck) highlighted the importance of keeping training and documentation agile:
“We spent a full year testing our approach to Modular Content. What we learned is that you don’t need to over-document every detail. Keep training materials practical, focused, and adaptable.”
By focusing on what is necessary rather than overcomplicating processes, organizations can make training more effective, ensuring that modular content adoption remains a smooth and scalable transition.
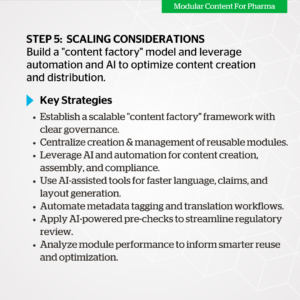
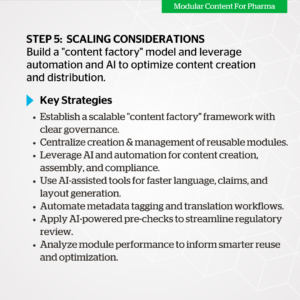
Step 5: Scaling Considerations
Building the Content Factory and Leveraging Automation
Once modular content has been piloted and adopted by key brands and markets, the next challenge is scaling. At this stage, the focus shifts from initial adoption to efficiencies at scale – a modular content “factory” model that combines process efficiency with intelligent automation to drive scale without compromising compliance or creativity.
A. Establish a Content Factory Model
A content factory is not a physical space – it’s a scalable operational framework that brings together modular processes, skilled resources, and enabling technology. It’s where volume meets velocity, and where modular thinking becomes embedded in everyday content creation.
Key elements of a pharma content factory:
- Centralized module creation and management with clear governance
- Pre-approved, reusable content elements for faster assembly and localization
- Design and layout templates aligned to different channels and use cases
- Defined roles and responsibilities across global, regional, and local teams
- A focus on quality, consistency, and compliance at every stage
This model allows content teams to efficiently serve diverse market needs while maintaining alignment to brand strategy and regulatory standards.
B. Embrace Automation and AI to Accelerate Scale
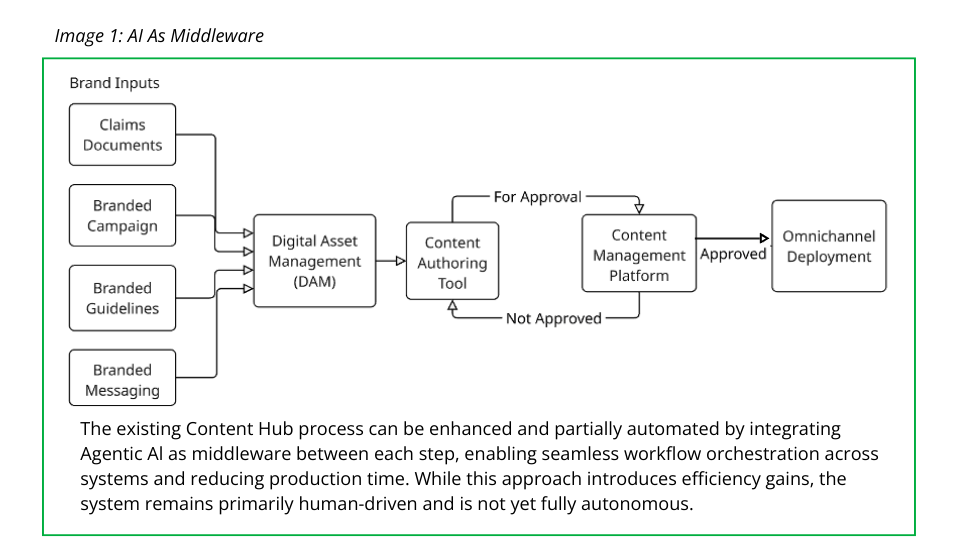
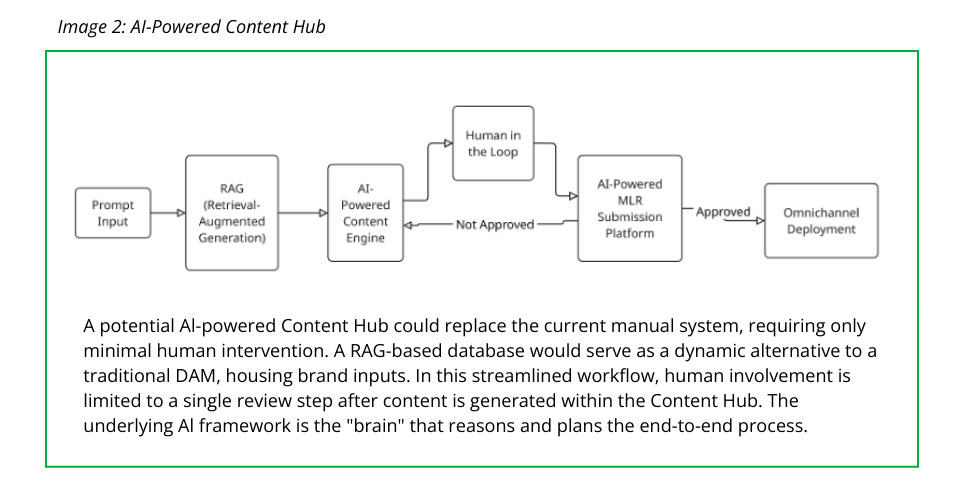
To truly unlock the potential of modular content, automation and AI must be leveraged across the content lifecycle—from creation to assembly, translation, and performance analysis. These technologies reduce manual effort, speed up approvals, and enhance personalization at scale.
Key automation and AI enablers:
- Generative AI (Gen AI) for generating original content elements like claims, CTAs, visuals, and headlines, as well as personalized variations for different audiences, channels, or markets. This speeds up content development and supports scalable personalization while staying aligned with brand and regulatory guidelines.
- AI-assisted authoring tools that recommend language, claims, or layouts based on approved assets
- Automated tagging and metadata assignment to ensure accurate and scalable content organization
- Rules-based content assembly engines that dynamically create emails, websites, or presentations using approved modules
- Translation memory systems that reuse prior translations for rapid localization
- AI-powered MLR pre-checks that proactively flag potential compliance issues – such as unsupported claims, off-label language, or missing references – before content reaches formal review, helping reduce back-and-forth cycles and speed time to approval
- Performance analytics that attribute engagement to specific modules, enabling smarter content reuse
By coupling modular foundations with the right AI tools, pharma companies can move from linear production to dynamic, on-demand content delivery.
Conclusion
Modular content holds transformative potential to reduce content development costs while driving personalization and efficiency. The proof is in the results early adopters have achieved. According to Hassan, “With modular content, we gain better consistency in messaging, improved traceability, and real insights into what content is resonating. Instead of just tracking clicks, we now understand how specific content elements perform…we’ve seen a 20-25% reduction in agency costs and up to 40% reduction in content creation time. Some emails that used to take over a week now take just 30 minutes to finalize.”
Implementing a modular content strategy in pharma is complex but achievable with the right approach. By integrating the main steps described in this article, pharma companies can achieve greater efficiency, compliance, and personalization.
Authors
Gregg Fisher, Managing Partner, The Stem – gfisher@thestem.com
Pedro Santos is a Lead Strategy Consultant, The Stem
with contributions from Joe Falcone and Stephanie Taubin, The Stem
Read the full post. +









 The pre-launch phase of the drug development process is arguably the most data- and stakeholder-intensive, lending itself to the benefits of AI. From protocol designs to site selection and management, patient recruitment and retention to drug supply management and adverse event reporting, data collection and analysis to risk management, the sheer volume of data and touchpoints can be overwhelming. Given the magnitude, it should come as no surprise that chatbots have already been used in this context for years.
The pre-launch phase of the drug development process is arguably the most data- and stakeholder-intensive, lending itself to the benefits of AI. From protocol designs to site selection and management, patient recruitment and retention to drug supply management and adverse event reporting, data collection and analysis to risk management, the sheer volume of data and touchpoints can be overwhelming. Given the magnitude, it should come as no surprise that chatbots have already been used in this context for years.  Jennifer Riggins, medical affairs thought leader and expert in medical communications and digital solutions, agrees. “Healthcare professionals don’t have a lot of trust when they don’t know where your clinical answers come from. I’ve seen criticisms around authorship, the belief that robots can’t be an author of scientific papers, or even clinical trial results. So, in addition to only pulling from a closed data set, make sure sources are cited, every claim and detail thoroughly and precisely referenced. Trust is largely based on transparency.”
Jennifer Riggins, medical affairs thought leader and expert in medical communications and digital solutions, agrees. “Healthcare professionals don’t have a lot of trust when they don’t know where your clinical answers come from. I’ve seen criticisms around authorship, the belief that robots can’t be an author of scientific papers, or even clinical trial results. So, in addition to only pulling from a closed data set, make sure sources are cited, every claim and detail thoroughly and precisely referenced. Trust is largely based on transparency.” Toon De Baere, senior director digital customer engagement Europe/Canada at AstraZeneca, has a similar vision. “Imagine all pharmaceutical companies providing important clinical information for their products, housed in a centralized, company-agnostic database. Physicians, liaisons, even patients could connect using an interface that independently answers their questions, provides resources, and helps manage these customer engagement relationships. The data would be open-ended, but all pre-approved and compliant.”
Toon De Baere, senior director digital customer engagement Europe/Canada at AstraZeneca, has a similar vision. “Imagine all pharmaceutical companies providing important clinical information for their products, housed in a centralized, company-agnostic database. Physicians, liaisons, even patients could connect using an interface that independently answers their questions, provides resources, and helps manage these customer engagement relationships. The data would be open-ended, but all pre-approved and compliant.” The potential for improved patient and caregiver engagement seems even more exciting. “In essence, you will not need a patient support program anymore, because your ChatGPT solution would be your patient support program,” Da Baere explains. “All the support resources could be available through the bot, making a website far less engaging, and essentially redundant.” Da Baere also speculates that actual conversations could populate the bot, thereby helping to formulate answers to difficult care questions that are expressed consistently, naturally, and empathetically.
The potential for improved patient and caregiver engagement seems even more exciting. “In essence, you will not need a patient support program anymore, because your ChatGPT solution would be your patient support program,” Da Baere explains. “All the support resources could be available through the bot, making a website far less engaging, and essentially redundant.” Da Baere also speculates that actual conversations could populate the bot, thereby helping to formulate answers to difficult care questions that are expressed consistently, naturally, and empathetically.